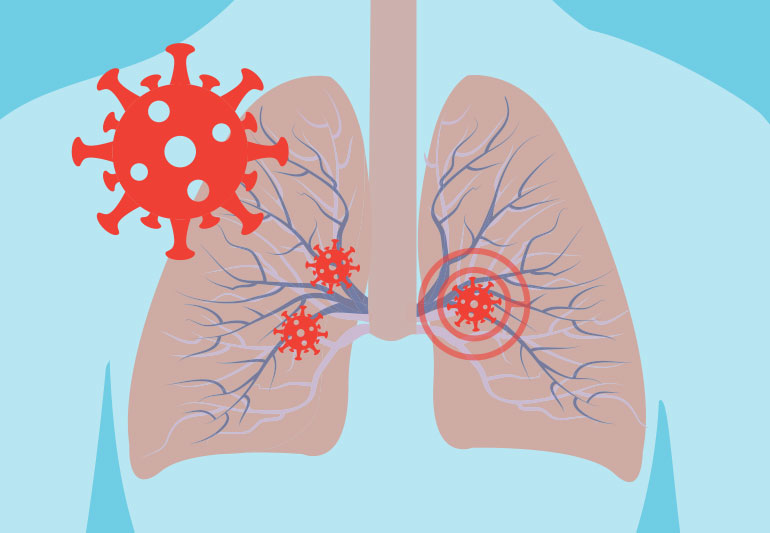
What Coronavirus Does to the Lungs
It is not news by now that the novel coronavirus, COVID-19, causes damage to the respiratory system. Questions like how and why, have a clearer understanding on the mechanisms in which the virus works than we did when the outbreak broke out earlier in the year.
In a John Hopkins University BLOG featuring Panagis Galiatsatos, M.D., M.H.S., an expert on lung disease at Johns Hopkins Bayview Medical Center that sees patients with COVID-19. He explains some of the short and long-term lung problems brought on by the new coronavirus.
The main types of respiratory damage caused by COVID-19 are pneumonia, ARDS, Sepsis, and superinfection;
Pneumonia – affects the lungs become filled with fluid and inflamed, leading to breathing difficulties. When cases become severe a ventilator is required when a patient must be intubated with a breathing apparatus. However, most people recover from pneumonia without any permanent lung damage, the pneumonia associated with COVID-19 may be severe. Even after the disease has passed, lung injury may result in breathing difficulties that might take months to improve according to Dr. Galiatsatos.
ARDS – The air sacs become filled with fluid leaking from the tiny blood vessels in the lungs which can create onset of shortness of breath. ARDS can be fatal. People who survive ARDS and recover from COVID-19 may have lasting pulmonary scarring.
Sepsis – is when bacteria circulate in the bloodstream creating massive amounts of systemic damage to organs and tissues. Sepsis, even when survived, can leave a patient with lasting damage to the lungs and other organs.
Superinfection – Galiatsatos notes that when a person has COVID-19, the immune system is working hard to fight the invader. This can leave the body more vulnerable to infection with another bacterium or virus on top of the COVID-19 — a superinfection. More infection can result in additional lung damage.
Three Factors in Coronavirus Lung Damage
Dr. Galiatsatos notes three factors that affect the lung damage risk in COVID-19 infections and how likely the person is to recover and regain lung function:
- Disease severity. “The first is the severity of the coronavirus infection itself — whether the person has a mild case, or a severe one,” Galiatsatos says. Milder cases are less likely to cause lasting scars in the lung tissue.
- Health conditions. Galiatsatos says, “The second is whether there are existing health problems, such as chronic obstructive pulmonary disease (COPD) or heart disease that can raise the risk for severe disease.” Older people are also more vulnerable for a severe case of COVID-19. Their lung tissues may be less elastic, and they may have weakened immunity because of advanced age.
- Treatment. “Treatment is the third factor,” he says. “A patient’s recovery and long-term lung health is going to depend on what kind of care they get, and how quickly.” Timely support in the hospital for severely ill patients can minimize lung damage.
Can patients lessen the chance of lung damage?
There are things patients can do to increase their chances for less severe lung damage, Galiatsatos says.
“If you have a health issue that puts you at higher risk, make sure you’re doing everything you can to minimize that. For example, people living with diabetes, COPD or heart disease should be especially careful to manage those conditions with monitoring and taking their medications as directed.”
Galiatsatos adds that proper nutrition and hydration can also help patients avoid complications of COVID-19. “Staying well fed is important for overall health. Proper hydration maintains proper blood volume and healthy mucous membranes in the respiratory system, which can help them better resist infection and tissue damage.”
Is COVID-19 lung damage reversible?
After a serious case of COVID-19, a patient’s lungs can recover, but not overnight. “Recovery from lung damage takes time,” Galiatsatos says. “There’s the initial injury to the lungs, followed by scarring. Over time, the tissue heals, but it can take three months to a year or more for a person’s lung function to return to pre-COVID-19 levels.”
He notes that doctors and patients alike should be prepared for continuing treatment and therapy.
“Once the pandemic is over, there will be a group of patients with new health needs: the survivors. Doctors, respiratory therapists and other health care providers will need to help these patients recover their lung function as much as possible.”
The severity of COVID-19 still remains a threat to the most vulnerable population with those with co-morbidities. Keep you and your family safe by learning your COVID-19 status by booking a COVID-19 one of many of the tests available at LabFinder.
References: https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/what-coronavirus-does-to-the-lungs

Andy Alem
The LabFinder Editorial Team is behind The Illuminator and The Insider, LabFinder’s consumer and business blogs.
Dr.Robert Segal
Dr. Segal is CEO and co-founder of LabFinder, as well as a board-certified cardiologist. He began practicing medicine in 2002 and has founded several businesses, including Medical Offices of Manhattan and Manhattan Cardiology.